http://www.physio-pedia.com/Lumbar_Spine_Fracture
Lumbar Spine Fracture
Original Editors - Thomas Albaugh, Elizabeth Record, Misty Hillin and Patrick Bales as part of theTexas State University's Evidence-based Practice project
Lead Editors
Lead Editors
Contents[hide] |
Definition/Description
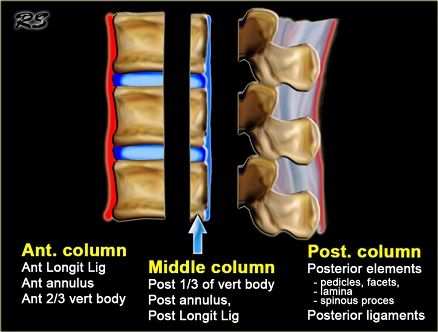
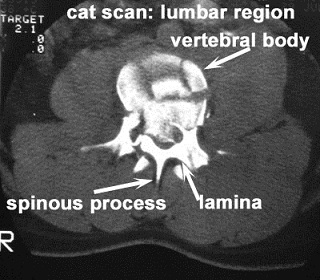
The complex shape of the vertebrae, along with the interaction of central nervous system, the relatively specialized structures of theintervertebral disks and the associated vertebral ligaments has made the description and classification of spinal fractures an ongoing pursuit for the medical community. The current system had its roots in 1963 after Holdsworth proposed classifying spinal fractures by the mechanism of injury (MOI) of compression, flexion, extension, and flexion-rotation. He divided the injuries involvement of the anterior weight bearing column and the posterior “tension bearing” column of facet joints and ligament complex[1].
The 1983 Denis system revision led to a center column comprised of the posterior vertebral body, posterior vertebral disk and posterior ;ongitudinal ligament[2].
Definition/Description
The complex shape of the vertebrae, along with the interaction of central nervous system, the relatively specialized structures of theintervertebral disks and the associated vertebral ligaments has made the description and classification of spinal fractures an ongoing pursuit for the medical community. The current system had its roots in 1963 after Holdsworth proposed classifying spinal fractures by the mechanism of injury (MOI) of compression, flexion, extension, and flexion-rotation. He divided the injuries involvement of the anterior weight bearing column and the posterior “tension bearing” column of facet joints and ligament complex[1].
The 1983 Denis system revision led to a center column comprised of the posterior vertebral body, posterior vertebral disk and posterior ;ongitudinal ligament[2].
In the Denis system it was believed that trauma focused into the middle column was sufficient to cause instability in the spine. The instability was further categorized into three types:
- First degree: considered mechanical
- Second degree: neurological
- Third degree: combined mechanical/neurological
This system is still currently the favored method. The main frustration from the Denis method is that the inclusion of the middle column introduced a “virtual landmark” that isn’t really suitable for determining an injury type. A recently developed system by Aebi incorporates the two column method, combined with the method of injury, and the instability which may result in neurological compromise. This method can result in 27 subgroups of spinal fractures[3]. Obviously the classification of fractures is complicated and ongoing.
The American Academy of Orthopedic Surgeons website lists fractures based on the pattern of injury and in a simpler format:
- The flexion pattern contains compression fractures, and axial burst fractures.
- The extension pattern, which contains flexion/distraction (often called a chance fracture).
- The rotation pattern contains transverse process and fracture-dislocation.[4]
While the listed examples above all imply trauma for a spinal fracture, osteoporosis and conditions such as osteogenesis imperfectaare commonly implicated in vertebral fractures as well.
Epidemiology /Etiology
Vertebral fractures detected with patients presenting with back pain account for only a third of osteoporitic fractures.[5]
The extension pattern of lumbar fractures:
- A chance fracture results from a distraction accident such as stopping quickly and the force from a seatbelt pulling the vertebrae apart.
The flexion pattern of lumbar fractures:
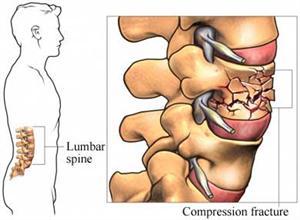
- Compression fractures are usually caused by an axial load that causes the anterior vertebrae to lose height.[4] Axial Burst fractures are caused by an axial load of a sudden acceleration or deceleration transmitted through the spine that causes the vertebrae to lose height on all sides.
- Burst fractures may result in some retropulsion of the vertebra into the vertebral canal.[6] Compression and burst fractures are most commonly seen in falls and traffic accidents.[6]
The rotation pattern of lumbar fractures:
- Transverse process (TP) fractures are uncommon and result from extreme sideways bending. These do not usually affect stability.
- The fracture-dislocation is a fracture in which bone and its accompanying soft tissue will move off an adjacent vertebra. This type is an unstable fracture and may cause severe spinal cord compression.
Characteristics/Clinical Presentation
Fractures of the lumbar spine and at the thoracolumbar junction are quite common. Per definition, in compression type fractures the anterior column is affected, whereas in burst fractures, anterior and middle column and sometimes the posterior column, are involved. Compression type fractures are predominately caused by indirect hyperflexion and bending forces whereas burst type fractures result from axial loading.[7]
More than 65% of vertebral fractures may not cause recognizable symptoms and may be undiagnosed with radiographs.[5] Patients could have neurologic involvement, may have low back pain, movement may be impaired, or a combination of all of them. When the spinal cord is also involved, numbness, tingling, weakness, or bowel/bladder dysfunction may occur.[4]
Upon inspection of the spine, the patient typically has a kyphotic posture that cannot be corrected. The kyphosis is caused by the wedge shape of the fractured vertebra; the fracture essentially turns the lateral conformation of the vertebra from a square to a triangle.[8]
Examination
Radiologists should take a proactive role in helping to diagnose spinal fractures. The failure to diagnose vertebral fracture is a worldwide problem due in part to the lack of fracture recognition by radiologists and the use of ambiguous terminology in radiology reports.[9]
Physical therapists can also be more engaged through a thorough exam that includes:
- A detailed history
- A neurological exam
- Palpation, especially midline along the vertebrae[8]
- ROM, STR, joint mobility and muscle length assessments
- Careful differential diagnosis
Medical Management (current best evidence)
Operative
- When neurological impairments are present, surgical procedures are usually required to repair or relieve the site of injury.[10]There are several procedures determined by the degree of compromise, the spinal level of the fracture and the patient's previous health status.[8]
Anterior/Posterior Approach:
- Often dictated by the severity of compromise or level of injury, a surgeon will make an anterior or posterior approach to the patient's spine in order to stabilize it. Rods, screws and other mechanical devices are inserted through remaining structures to fuse the affected vertebra(e). The anterior approach dominates upper lumbar (L1, L2) fractures due to involvement with the crura of the diaphragm while lower lumbar fractures (L5) are stabilized through a posterior approach method.[11][12]
Kyphoplasty:
- A mini-invasive percutaneous procedure that relieves vertebral fracture pain through the heat discharged during bone cement coagulation. The cement also solidifies to further stabilize the site of injury.[13] During the procedure, a cannula is introduced into the vertebral body followed by a bone expander to regain some vertebral height. Kyphoplasty has been found to be similar in success rate as vertebroplasty, but with greater recovery of vertebral height.[14]
Vertebroplasty:
- An effective treatment in the management of vertebral compression fractures, vertebroplasty involves injecting bone fillers such as polymethylmethacrylate (PMMA) bone cement into the fractured vertebral body.[14][15]
Non-operative
Patients not requiring surgery receive treatments that target pain relief with bracing and rehabilitiation therapy.[8] Those with compression type and burst type fractures involving the anterior and middle column have been described as the best candidates for non-operative management.[7] A thoracic-lumbar-sacral orthosis (TLSO) is the current brace of choice for these types of injuries, however, patients will also want to move into mobility as their pain and healing process progresses. Thus allowing them to move into weight-bearing exercises to prevent future osteoporosis and extension exercises.[8]
Non-operative options are increasingly becoming the preferred method of fracture management as bracing and therapy methods are shown to be as clinically effective, yet much more cost efficient than surgical options. [16]
Pharmaceutical
Medications ranging from Tylenol and NSAIDS to opiods can be taken to modulate lumbar spine fracture pain. Spinal nerve blocks at the L2 region have also been found to be effective against acute low back pain from fractures.[17]
Physical Therapy Management (current best evidence)
The purpose of physical therapy management in patients with lumbar spine fracture is to decrease pain, increase mobility and prevent future occurances.[8] While mobility is important, back extensor and abdominal (core) strength have been shown an effective therapeutic intervention for those with lumbar problems associated with osteoporosis. In particular, the multifidus, quadratus lumborum and transverse abdominals help support the spine. So much so that increasing strength not only relieves pain and symptoms from those patients with fractures, but also can act as a preventative to decrease future fractures. Physical therapy programs that promote exercise targeting impairments in intrinsic back strength have been shown to improve the function and quality of life in those with osteoporotic vertebral fracture. [18][8][16]
This exercise works both the core and back muscles, hitting the TA, multifidus and quadratus lumborum.
Thoracolumbar fracture therapy evidence closely parallels that of the lumbar spine and other exercises can be seen hereThoracic_Spine_Fracture.
Overall, physical therapy has been shown to have no clinical significant difference in outcomes when compared to surgery for appropriate spinal fracture patients. Not only does physical therapy help relieve pain and disability as well as surgery, but the overall cost to the patient is greatly reduced.[16]
Resources
Clinical Bottom Line
Lumbar spine fractures, whether from an acute injury or progressive in nature like osteoporosis, occur often enough to merit adequate research with regard to healing procedures. A great deal of inquiry has gone into spinal surgery options, while very little appears to exist for specific physical therapy management. Most of the present information acknowledges that physical therapy, especially that of therapy and bracing can just as effectively manage lumbar fracture pain (without neurological involvement) as that of surgery. However, no current research exists that effectively compares the most effective therapy. Current recommendations revolve around basic core and lumbar spine strengthening as with most lumbar spine insults. It is our recommendation that more research be done in this area that focuses specifically on lumbar spine fractures and the most effective therapy treatments for these injuries.
Recent Related Research (from Pubmed)
- Location of Sternal Fractures as a Possible Marker for Associated Injuries.
- Bisphosphonates for the prevention and treatment of osteoporosis in patients with rheumatic diseases: a systematic review and meta-analysis.
- Bone disease in systemic sclerosis: outcomes and associations.
- Infection with Bacteroides thetaiotaomicron during Posterior Decompression and Dynamic Stabilization of the Lumbar Spine: A Case Report and Review of the Literature.
References
- ↑ Holdsworth FW. Fractures, dislocations and fracture/dislocation of the spine. J Bone Joint Surg Br 1963;45:6-20.
- ↑ Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine 1983;8:817-31.
- ↑ Aebi M. Classification of thoracolumbar fractures and dislocations. Eur Spine J 2009;19:(suppl I):S2-S7.
- ↑ 4.0 4.1 4.2 American Academy of Orthopaedic Surgeons (AAOP). http://orthoinfo.aaos.org/topic.cfm?topic=a00368 (accessed 27 April 2011).
- ↑ 5.0 5.1 Lentle B, Brown J, Hodsman A, et al. Recognizing and Reporting Vertebral Fractures: Reducing the Risk of Future Osteoporotic Fractures. Canadian Association of Radiologists Journal [serial online]. February 2007;58(1):27-36. Available from: Academic Search Complete, Ipswich, MA. Accessed May 1, 2011.
- ↑ 6.0 6.1 Heary R, Kumar S. Decision-making in burst fractures of the thoracolumbar and lumbar spine. Indian Journal of Orthopaedics [serial online]. October 2007;41(4):268-276. Available from: Academic Search Complete, Ipswich, MA. Accessed April 14, 2011.
- ↑ 7.0 7.1 Weninger P, Schultz A, Hertz H. Conservative management of thoracolumbar and lumbar spine compression and burst fractures: functional and radiographic outcomes in 136 cases treated by closed reduction and casting. Archives of Orthopaedic &Trauma Surgery [serial online]. February 2009;129(2):207-219. Available from: Academic Search Complete, Ipswich, MA. Accessed April 14, 2011.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Sherman AL, Razack N, Slipman CW et al. Lumbar Compression Fracture. Medscape Reference. Available athttp://emedicine.medscape.com/article/309615-overview. Accessed April 25, 2011.
- ↑ Lenchik L, Rogers LF, Delmas PD, et al. Diagnosis of Osteoporotic Vertebral Fractures: Importance of Recognition and Description by Radiologists. Am J Roentgenol Radium Ther Nucl Med. 2004;183:949-58.
- ↑ Yi L, Jingping B, Gele J, Wu T, Baoleri X. Operative versus non-operative treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD005079. DOI: 10.1002/14651858.CD005079.pub2.
- ↑ Selznick LA, Shamji MF, Isaacs RE. Minimally invasive interbody fusion for revision lumbar surgery: technical feasibility and safety. J Spinal Disord Tech. May 2009;22(3):207-13.
- ↑ Benzel EC, Ball PA. Management of low lumbar fractures by dorsal decompression, fusion, and lumbosacral laminar distraction fixation. J Neurosurg 2000;92(2 Suppl):142-8.
- ↑ Xiong J, Dang Y, Jiang B et al. Treatment of osteoporotic compression fracture of thoracic-lumbar vertebrae by kyphoplasty with SKY bone expander system. Chinese J Traumatol (English Edition) 2010;13(5):270-4.
- ↑ 14.0 14.1 Zhou J, Liu S, Ming J et al. Comparison of therapeutic effect between percutaneous vertebroplasty and kyphoplasty on vertebral compression fracture. Chinese J Tramatol (English Edition) 2008;11(1):42-4.
- ↑ Rapan S, Jovanovic S, Gulan G. Vertebroplasty for vertebral compression fracture. Coll Antropol 2009;33(3):911-4.
- ↑ 16.0 16.1 16.2 Stadhouder A, Buskens E, de Klerk LW et al. Traumatic Thoracic and Lumbar Spinal Fractures: Operative or Nonoperative Treatment: Comparison of Two Treatment Strategies by Means of Surgeon Equipoise. Spine 2008;33(9):1006-17.
- ↑ Ohtori S, Yamashita M, Inoue G, et al. L2 spinal nerve-block effects on acute low back pain from osteoporotic vertebral fracture. J Pain 2009;10(8):870-5.
- ↑ Bennell KL, Matthews B, Greig A, Briggs A, Kelly A, Sherburn M, Larsen J, Wark J. Effects of an exercise and manual therapy program on physical impairments, function and quality of life in people with osteoporotic vertebral fracture: A randomised, single-blind controlled pilot trial. BMC Musculoskeletal Disord 2010;11(36):1-11.

No hay comentarios:
Publicar un comentario